Definition
Diabetes Spectrum. January 2002 vol. 15 no. 1 28-36
CMAJ. 2003 Apr 1;168(7):859-66.
Diabetic ketoacidosis (DKA), the hallmark of type 1 diabetes mellitus (T1DM), and hyperglycemic hyperosmolar state (HHS), primarily seen in type 2 diabetes (T2DM), are hyperglycemic emergencies that may lead to death if untreated. They are both associated with:
-
- Insulin deficiency (absolute in T1DM and relative in T2DM) and hyperglycemia
- Acid-base abnormalities (ketoacidosis)
- Severe volume depletion
Euglycemic DKA
Diabetes Care. 2015 Sep; 38(9): 1687–1693.
DKA can very rarely occur with normal glucose levels, particularly in the setting of prior insulin use or pregnancy. This has been a known complication with the rise in the usage of SGLT2i (sodium glucose transporter type 2 inhibitors) class of medications. Renal wasting of glucose does not allow for serum glucose to rise to the levels seen in DKA and HHS.
Physiology and function of insulin
Curr Diabetes Rev. 2013 Jan 1; 9(1): 25–53.
Clin Biochem Rev. 2005 May; 26(2): 19–39.
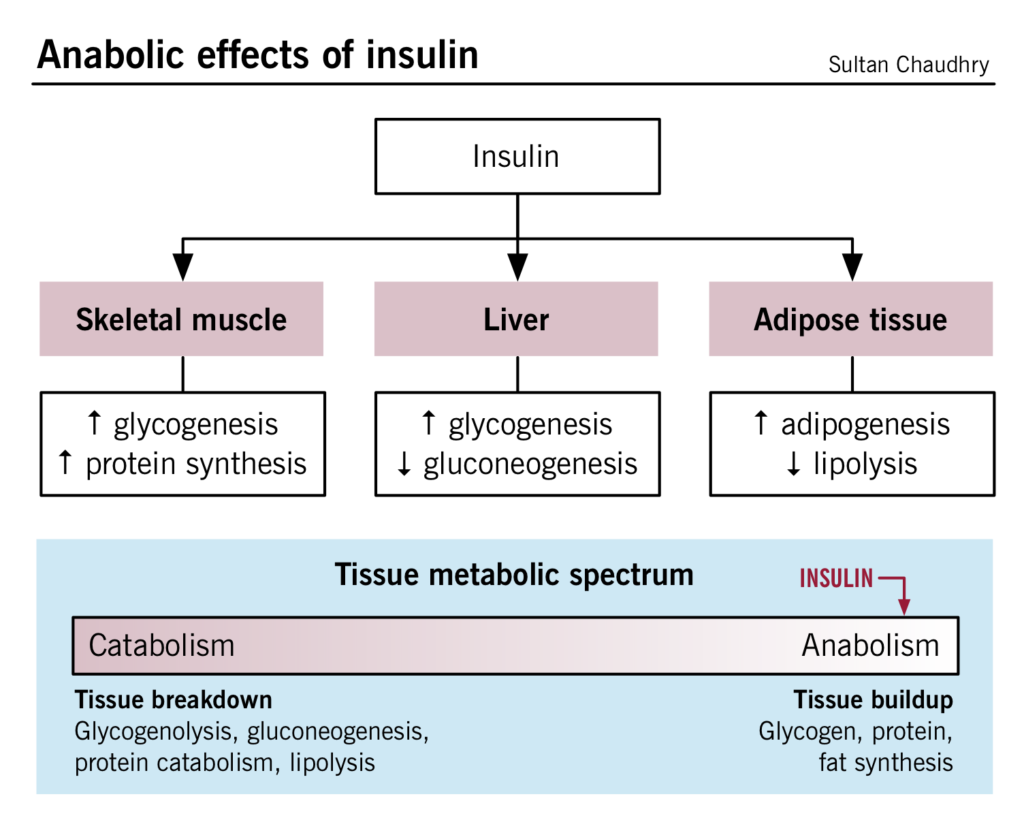
Insulin, a peptide hormone, is produced by the beta-islet cells in the pancreas. Major functions of insulin include increased glucose uptake by the peripheral tissues (liver, skeletal muscle and adipose tissue), enhancing glycogenesis, adipogenesis and inhibition of lipolysis and glycogenolysis. These functions are summarized in the flowchart below. Please see the Diabetes chapter (in preparation) for further details.
Pathogenesis and Pathophysiology
Metabolism. 2016 Apr;65(4):507-21
Endocrinol Metab Clin North Am. 2013 Dec;42(4):677-95
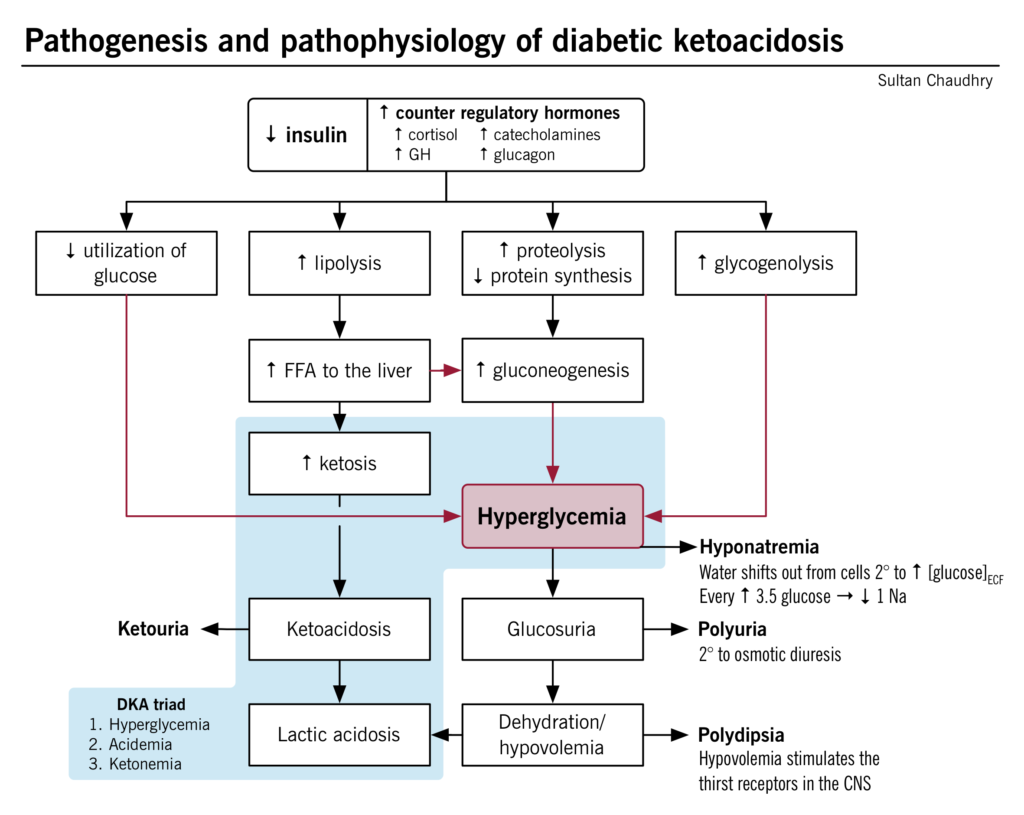
DKA is a result of an absolute or relative insulin deficiency, leading to ketoacidosis, volume depletion and hyperglycemia. Insulin is the primary anabolic hormone that allows peripheral tissues to uptake glucose. In the absence of insulin, the other counterregulatory hormones act together to break down triglycerides and stimulate gluconeogenesis. In DKA, the normal state of carbohydrate metabolism (driven by insulin) shifts to a starvation state and fat metabolism, leading to the characteristic abnormalities, including hyperglycemia, ketoacidosis, hyponatremia, polyuria, and polydipsia. Please see details of the pathophysiology outlined in the figure/flowchart below.
Metabolic Derangements of DKA vs. HHS
The insulin concentrations required for anti-lipolysis effects are lower than those required for glucose uptake by peripheral tissues. The circulating insulin in patients with HHS is enough to inhibit lipolysis and generation of ketone bodies.
The absolute deficiency of insulin causes severe ketosis and patients tend to be “sicker” and present earlier, than patients with HHS. Since HHS presents later, patients generally have more severe volume depletion and relatively worse hyperglycemia.
The precipitants for both are similar and are presented in the chart below, along with their mechanisms.
| Precipitants | Mechanism(s) |
| Infection | Increased metabolic demands and failure to increase insulin levels
Increase in the counterregulatory hormones (stress response) also further inhibits insulin release |
| Non-compliance with insulin regimen | Lack of insulin are unable to regulate the continuous intake of food and counterregulatory hormones are not inhibited. |
| First time presentation of T1DM | Deficiency of insulin and potentially other precipitants (infection). |
| Medical illness (MI, stroke, trauma, pancreatitis) | Higher metabolic demands
High counterregulatory hormone levels to compensate for the physiologic stress. Failure to raise insulin levels. |
Clinical & Laboratory Features
Endocrinol Metab Clin North Am. 2013 Dec;42(4):677-95
N Engl J Med 2015; 372:546-554
| Signs & Symptoms | Mechanism(s) |
| Confusion/Coma | Present in severe cases and has been thought to be related to the dehydration and acidemia. |
| Tachycardia and hypotension | Due to a state of severe intravascular volume depletion from the osmotic diuresis (glucosuria), vomiting (if associated), as well as ketoacidosis. |
| Fever | Could be present if etiology is infectious |
| Polydipsia and polyuria | See pathogenesis/pathophysiology figure above. |
| Kussmaul respiration (deep laboured breathing)/tachypnea | Respiratory response for the metabolic acidosis; an attempt to reduce the carbon dioxide levels in the blood (further reduction in acid concentrations).
H+ + HC03- → H2C03 → H20 + CO2 |
| Abdominal pain and tenderness | Mechanisms unknown but appears to be related to the metabolic acidosis. |
| Nausea and vomiting | Related to ketoacidosis (particularly beta-hydroxybutyrate, which has emetic properties), or maybe underlying precipitant of DKA. |
| “Sweet odor” | Acetone (one of the ketoacids) can sometimes be subtly smelled in the patient’s breath. |
| Lab Finding(s) | |
| Hyperglycemia, Acidemia (pH<7.3) | See pathogenesis/pathophysiology figure above. |
| Hyponatremia | Secondary to hyperglycemia. Correction factor: For every 3.5mmol/L rise in glucose, 1mmol/L should be added to the lab sodium value |
| Glucosuria | See pathogenesis/pathophysiology figure above.
Filtered glucose in the glomerulus is reabsorbed via the sodium glucose transporter (SGLT2), in the proximal convoluted tubule. The renal threshold for glucose absorption is exceeded, in the circumstances of severe hyperglycemia, resulting in glucosuria. |
| Ketonemia and ketonuria | Secondary to lipolysis and increase free fatty acid production. |
Treatment
Endocrinol Metab Clin North Am. 2013 Dec;42(4):677-95,
Diabetes Metab Syndr Obes. 2014; 7: 255–264.
Emerg Med Clin North Am. 2014 May;32(2):437-52
The principles of therapy are to (i) investigate and correct the underlying precipitant, (ii) replace fluid loss, and (iii) correct metabolic abnormalities. A protocolized approach to management with a flowsheet will ensure timely interventions and avoid errors. Inappropriate resuscitation might lead to worsening acidemia, shock, severe end organ damage including coma and death, Immediate volume resuscitation is important along with close monitoring of serum glucose, pH, bicarbonate as well as serum electrolytes to ensure improvement and monitoring for complications.
- IV fluid replacement:
- The initial management of DKA consists of initiating IV fluid replacement.
- This allows the body to utilize more glucose in the periphery (increased perfusion).
- Also helps to correct dehydration and lactic acidosis, restoring end organ perfusion and halting the progressive acidosis.
- Insulin:
- Inhibits the continuous lipolysis/ketosis and the release of counterregulatory hormones inducing DKA.
- Stimulates glucose uptake by the peripheral tissues (an attempt to normalize glucose levels)
- Reverses the acidosis.
- Patients should be safely transitioned to subcutaneous insulin therapy once the anion gap has normalized or patient is able to tolerate oral intake.
- Avoid/management of the complications
- Hypokalemia: Insulin stimulates the transcellular transport of potassium and can lead to hypokalemia, therefore IV potassium is replaced with the insulin infusions.
- Initially potassium levels can be normal or even high due to the hyperosmolarity and the dehydration. Potassium loss occurs with the glycosuria.
- Hypoglycemia: Continues insulin infusions can sometimes take the glucose levels below normal, however, can be easily managed by starting a D5W or D10W infusion.
- Cerebral edema: Due to continuous IV hydration (hypothesized to be secondary to rapid decline in plasma osmolality with treatment that results in an efflux of water into brain cells), cerebral edema can develop (more common in children).
- Mannitol, an osmotic diuretic can be given, if cerebral edema is suspected.
- Pulmonary edema: Hypothesized to be secondary to aggressive fluid resuscitation.
- Thrombosis: Hypothesized to be secondary to hypercoagulability due to volume depletion.
- Hypophosphatemia: Hypophosphatemia can occur due to renal wasting along with glucosuria but treatment is not recommended unless severe hypophosphatemia is present or there are concern cardiac arrhythmias present.
- Hypokalemia: Insulin stimulates the transcellular transport of potassium and can lead to hypokalemia, therefore IV potassium is replaced with the insulin infusions.
- Treat underlying precipitant:
- Treat respective of the etiology.
- Bicarbonate: Bicarbonate therapy has not been shown to be of any benefit in patients with DKA, and is generally only recommended in patients with severe acidemia (pH < 6.9).