Definition
- Bronchiolitis is the most common lower respiratory illness in children younger than 2. Viral infection, most often with Respiratory Syncytial Virus (RSV) is responsible for inflammation of the respiratory tree, particularly the bronchioles. Both upper and lower respiratory tract symptoms are seen in this illness which, for most previously healthy patients, is a self-limited and requires only supportive care.
Epidemiology
Pediatr Rev. 2009 Oct;30(10):386-95
- Incidence peaks during the winter months (December to March) when RSV is most prevalent.
- The most common risk factor for hospital admission is age, with most patients admitted for bronchiolitis being younger than 12 months.
Etiology
- The most common pathogen is respiratory syncytial virus (RSV), which accounts for 50-75% of all acute bronchiolitis cases. RSV is the most common respiratory pathogen worldwide; virtually all children have been infected by the age of 2. Other pathogens include adenovirus, rhinovirus, human metapneumovirus, influenza virus and parainfluenza virus.
- Transmission of RSV is by droplet and direct contact of respiratory secretions.
- Clinical infection is preceded by a latent period of 4-6 days.
- RSV is highly contagious among both adults and children, but infections in infants cause significant illness due to underdevelopment of immune defenses and smaller airway diameter; even small decreases in diameter caused by inflammation and secretions can impair laminar airflow and cause respiratory distress (recall Poiseuille’s law, which describes resistance as inversely proportional to radius to the power of 4).
Risk factors
Pediatr Rev. 2009 Oct;30(10):386-95
Pediatr Rev. 2012 Jun;33(6):255-63.
Pediatrics. 2007 Oct;120(4):e1076-81.
Pediatr Rev. 2012 Jun;33(6):255-63.
Pediatrics. 2007 Oct;120(4):e1076-81.
- Most cases of bronchiolitis occur in previously healthy children, and the major risk factor for these patients is contact with other children (e.g. daycare).
- Risk factors for serious illness include prematurity, congenital heart disease, lung disease and immunodeficiency.
- Prematurity: Alveolarization occurs at ~36 weeks gestation, and mature surfactant production by type II pneumocytes begins at 34-35 weeks. Premature infants are therefore born with immature lungs that are unprepared for normal gas exchange, and are at risk for developing Chronic Lung Disease (CLD). CLD results from dysplastic lung maturation secondary to a number of conditions, both as a part of the natural history of prematurity, as well as iatrogenic causes. These include prolonged ventilation with high oxygen concentrations and inspiratory pressures, inflammation, and infection. Infants and children who were premature and have CLD are at increased susceptibility to more severe respiratory infections.
- Congenital heart disease: Unrepaired or hemodynamically significant CHDs that have associated pulmonary overcirculation, which may involve baseline pulmonary edema or pulmonary hypertension, are at increased risk for more severe respiratory symptoms.
- Airway abnormalities: Children with laryngomalacia, tracheomalacia, and cleft lip or palate may have difficulty managing increased upper airway secretions.
- Down syndrome: DS has been identified as an independent risk factor for RSV infection, particularly infection requiring hospital admission. The increased risk may be, at least in part, due to CHD (present in ~50% of children with DS), pulmonary hypertension (found in 10% who do not have CHD), abnormal upper airway physiology contributing to apnea and difficulty clearing secretions, and immune response alterations (abnormal thymus development and function, low B and T cell numbers).
- Children with the above risk factors should be assessed for eligibility for RSV prophylaxis with palivizumab, an RSV-specific monoclonal antibody that has been shown to decrease hospitalization rate in high-risk children.
Pathogenesis
J Matern Fetal Neonatal Med. 2013 Oct;26 Suppl 2:55-9.
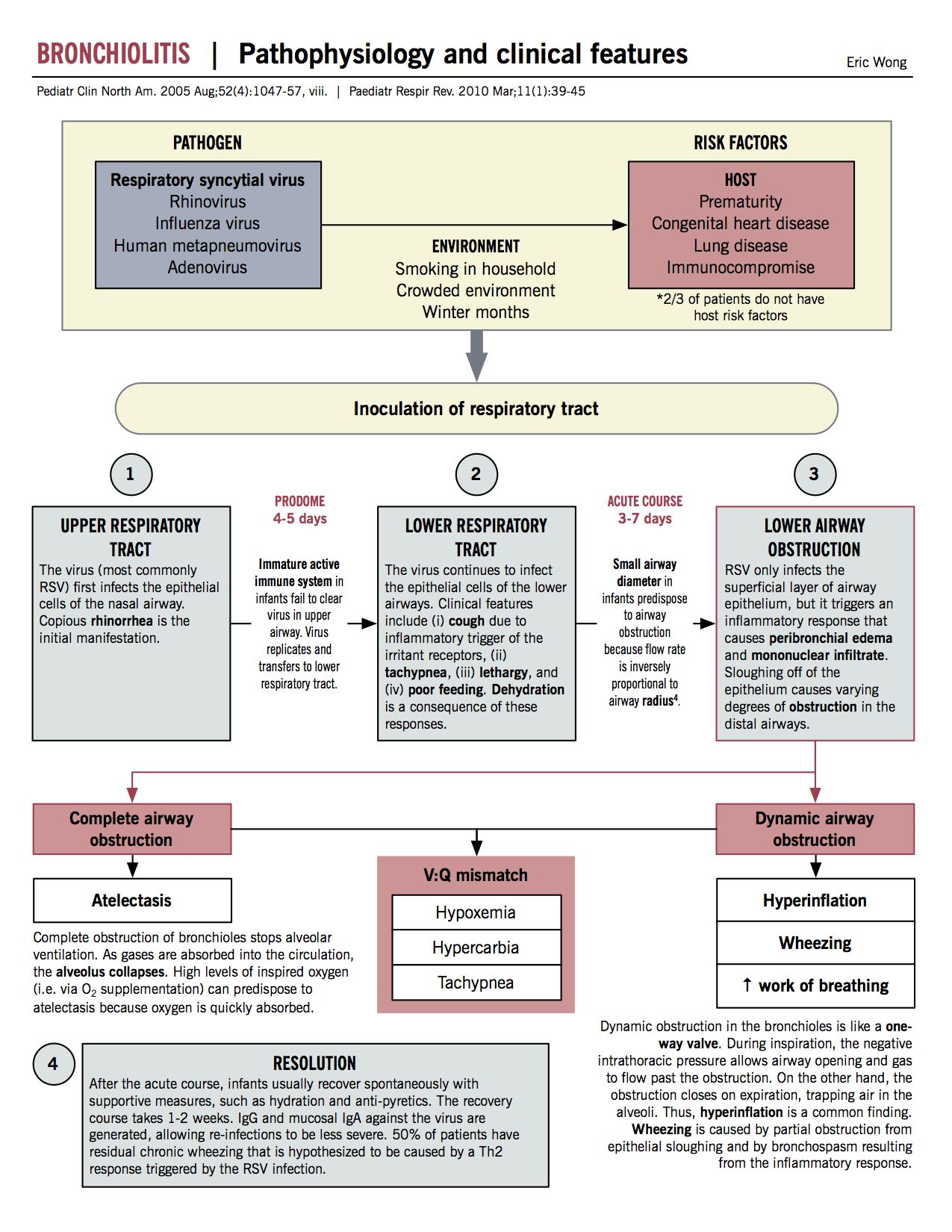
- Direct viral inoculation of respiratory epithelium leads to inflammation of small airways. The mechanisms by which RSV spreads along the respiratory tract are still not fully known, but likely include cell-to-cell transfer along intracytoplasmic bridges or aspiration of nasopharyngeal secretions.
- RSV can also damage cells of the structural airway and impair immune cells residing in the lungs.
- The host’s inflammatory response contributes to the pathophysiology and symptomatology: Host cells recognize RSV via toll-like receptors, and secrete inflammatory cytokines (e.g. IFN-γ, IL-1β, IL-4, IL-8). These effectors influence the local tissue environment directly, and also further the inflammatory process by drawing immune cells from the periphery. Many cytokines have known roles in the pathogenesis of RSV bronchiolitis, and some are even implicated in sustaining the infection. For example, the helper T cell’s main cytokine, IL-17, enhances RSV infection by increasing mucus production, inhibiting CD8 T cell activation, and reducing viral clearance.
Clinical features
Pediatr Rev. 2009 Oct;30(10):386-95
- The first signs and symptoms of bronchiolitis (and in many children, the extent of disease manifestations) are those of an upper respiratory tract infection:
- nasal discharge and congestion
- fever
- decreased appetite
- decreased energy, irritability
- In up to 30% of infected children younger than 2, there is extension of the infection into the lower airways. Cough, tachypnea and and increased respiratory effort follow the upper airway prodrome. Lower tract involvement ranges in severity, from mild to life-threatening respiratory failure.
- In very young infants, especially those who have a history of prematurity, apnea may be the sole presenting sign. Infants may also have copious production of secretions.
- The most clinically significant parameters in determining illness severity are respiratory rate, work of breathing, and hypoxia.
| Signs and symptoms | Mechanism(s) |
| Rhinorrhea, cough | Viral infection leads to irritation and inflammation of mucosal tissues |
| Tachypnea and increased work of breathing | Infection of lower airways results in inflammation, causing airway obstruction, decreasing effective gas exchange and causing ventilation-perfusion mismatch |
| Crackles/wheezing | Lower airway inflammation leads to collapse of smaller alveoli, leading to crackles heard on auscultation. Intrathoracic obstruction causes airway collapse during expiration, leading to wheezing. |
Natural history
- The course of bronchiolitis follows a characteristic pattern. Symptoms peak at around day 3 to 4 of illness.
- Most infections resolve with supportive treatment over 1-2 weeks.
- As previously mentioned, complications are more likely to occur in premature infants, neonates, patients with underlying heart or lung disease, and immune disorders. Common acute complications in infants include apnea, poor feeding, and dehydration. In those with underlying cardiorespiratory disease, complications include prolonged oxygen requirements, respiratory failure, intubation, and heart failure. Patients with compromised or deficient immune defenses may develop severe infection leading to respiratory failure, or superimposed bacterial infection.
- The most common long-term complication is recurrent wheezing episodes, especially with subsequent viral infecitions. Of infants diagnosed with bronchiolitis, approximately 40% will have wheezing episodes up to age 5, and 10% will continue to have wheeze after age 5. The relationship between bronchiolitis and recurrent wheeze remains unclear; recent theories suggest that children who develop post-bronchiolitic wheeze may harbor a predisposition to both RSV infection and recurrent wheeze. Relevant aspects of this relationship are of ongoing study and include the complexity of the immune system, environmental factors including infectious agents, and genetics (i.e. atopy).
Pathophysiology
Pediatrics. 2006 Oct;118(4):1774-93.
Arch Pediatr Adolesc Med. 2004 Feb;158(2):119-26.
J Matern Fetal Neonatal Med. 2013 Oct;26 Suppl 2:55-9.
Arch Pediatr Adolesc Med. 2004 Feb;158(2):119-26.
J Matern Fetal Neonatal Med. 2013 Oct;26 Suppl 2:55-9.
Airway obstruction
Lower
- Dynamic airway obstruction leads to increased work of breathing and wheezing, while complete obstruction can lead to atelectasis.
- Either form contributes to ventilation-perfusion mismatch and resultant hypoxia, hypercarbia and tachypnea.
Upper
- Upper airway obstruction by mucous secretions, which may be copious, contributes to poor feeding and increased respiratory effort.
Diagnosis
- Diagnosis is made clinically on the basis of a thorough history and physical examination.
- Chest radiography is not required to confirm diagnosis unless pneumonia is equally suspected. Chest x-rays have been shown to increase the likelihood of overdiagnosis of pneumonia with subsequent use of antibiotics without difference in recovery time. Radiographic findings do not correlate well with clinical manifestations of disease. The appearance of bronchiolitis on a chest x-ray may include hyperinflation, and patchy opacification representing infiltrates and/or atelectasis.
- Nasopharyngeal swab (NPS) may be done for viral testing to confirm an infection and identify the specific virus, but this test does not change clinical decision making or outcomes. Many viruses can produce the same clinical presentation, and clinical signs guide isolation procedures, not virus type.
Treatment
Pediatr Rev. 2009 Oct;30(10):386-95
- The managements strategies for bronchiolitis are largely supportive, with hydration and oxygenation as the primary interventions
- Hydration: Intravenous fluids are often necessary to correct dehydration and maintain hydration in a child with poor oral intake secondary to their infection. Oral rehydration with preparations such as Pedialyte, which delivers electrolytes and carbohydrates, may be used if the child expresses interest in oral intake, but should be used with caution in children with significant work of breathing due to aspiration risk. Some infants may benefit from nasogastric feeding until feeding improves.
- Oxygen: Oxygen to maintain saturation >90-92%, delivered by an appropriate method (e.g. nasal prongs, rebreathing or nonrebreathing masks).
- Bronchodilators, inhaled epinephrine, corticosteroids, antiviral agents, antibacterial agents, chest physiotherapy, nasal suction and decongestant drops are therapies that have been and continue to be used in variable measure, but none have demonstrated significant impact on duration of illness, severity of clinical course, or subsequent clinical outcomes (e.g. postbronchiolitis wheezing). Many of these treatments are used in emergency department settings nonetheless, often on the basis that some therapies such as nasal suction or bronchodilator and/or epinephrine, may ease symptoms. Some sources suggest a trial of these therapies, with discontinuation in the absence of effect.
- Given the predictable course of bronchiolitis, the “day of illness” can guide changes to supportive care: a child on Day 4 who continues to have intermittent desaturation on pulse oximetry may not require continued oxygen therapy (as a child on Day 2 with the same clinical picture might).
Prevention/prophylaxis
- Hand washing and routine infection control practices remain crucial to prevention of infection spread, as well as to re-infection
- Breastfeeding, particularly of longer duration, seems to have protective effective
- Palivizumab (Synagis) prophylaxis for high risk patients (see above). This monoclonal RSV-specific antibody, given during peak RSV season, confers passive immunity to infants at high-risk for severe illness.
| Passive immunity | Acquired immunity |
‘Natural’ mechanisms
|
Relies on antigen presentation by antigen presenting cells (i.e. dendritic and B cells) to activate specific cell-mediated and humoral response |
Artificial mechanism
|
Memory B and T cells develop in response to infection |
| Short-term immunity | Long-term immunity |